- Home
- About Us
- Our Work
- Initiatives
- Disaster Relief
- Hospital and Clinic Projects & Support
- Education & School Support
- Refugee Support
- Healthcare Education & Outreach
- Healthcare Capacity Building & Health Systems Strengthening
- Mobile Clinic Outreach
- Economic Stability & Livelihood
- Community Support
- Psychological Trauma Support
- Health Research
- News & Updates
- Get Involved

Pakistan: Why Millennium Development Goal #5 IMPROVE MATERNAL HEALTH is unlikely to be reached by 2015
JANUARY 22, 2013 - PAKISTAN
by Dr Martina C. Fuchs: Here is a fascinating and sad study report from RMF’s research team in Pakistan that details why Pakistan, despite several MNCH (Maternal Newborn and Child Health) interventions for the past two decades is unlikely to meet the MDG goal # 5 by 2015.
For a detailed report: http://realmedicinefoundation.org/initiative/update/pakistan-disparities-to-access
By Dr Rubina Mumtaz
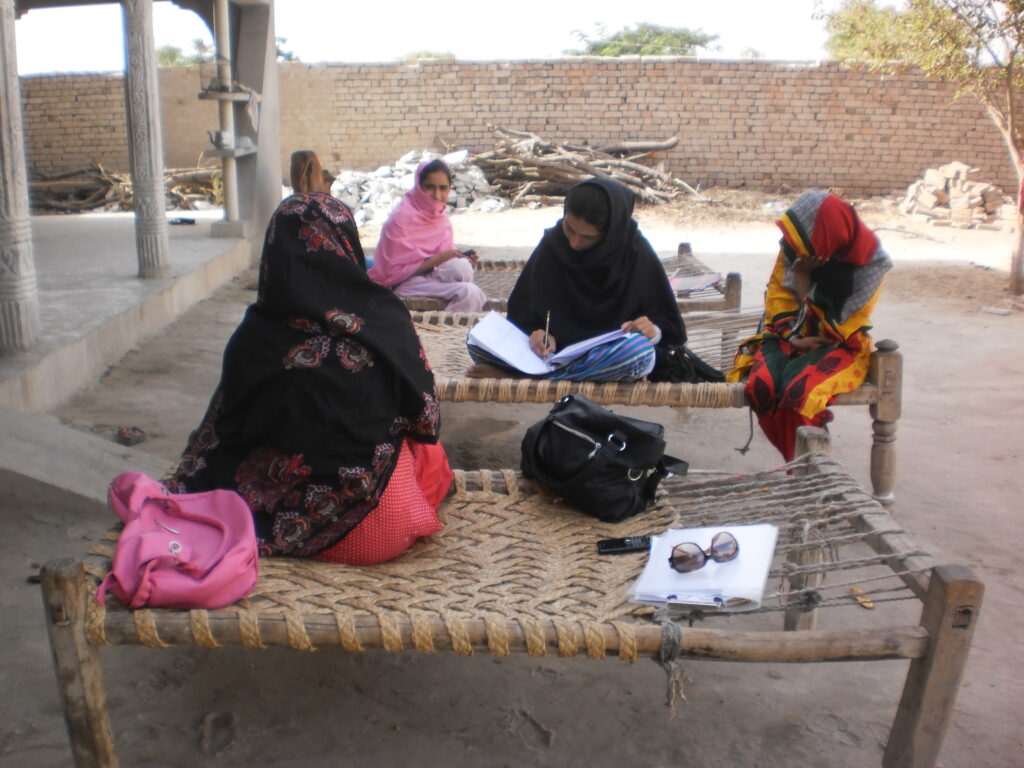
At the conversation session on “Disparities to Access to Maternal Health Services in Punjab; Poverty, Gender and Social Exclusion” held in Islamabad in November, the principal investigator, Dr Zubia Mumtaz, Faculty of School of Public Health, University of Alberta, shared the findings of the 10-month ethnographic study conducted in Chakwal district of Punjab that was funded by the Canadian Institute of Health Research (CIHR).
The background to the study research was that Pakistan, despite several MNCH interventions for the past two decades is unlikely to meet the MDG goal # 5 by 2015 because the focus is only on strengthening technical and managerial services in the public sector, such as increasing supply of services with a technical health systems approach or creating demand though health education.
The root causes of the inequities, in particular the social ‘causes of the causes’ in access to services remain neglected. Addressing this social aspect, the findings of the study identified the South Asian social caste system that promotes social exclusion as the key barrier to identifying and thus accessing disadvantaged and vulnerable women from the lowest social castes (Kammis), a group of people that contribute to 80% of MMR statistics in Pakistan. The average Kammi (comprising 20% of the population) works for the higher social classes on a ‘seph’ contract where remuneration for services is loosely defined such as small cash payments with occasional longer-term benefits e.g. land to build a house, major expenses including maternal health emergencies as well as social protection, a key element of security. The ‘seph’ contract is characterized by pervasive uncertainty; hence it leans towards chronic, intergenerational poverty. Yet Kammi poverty is NOT acknowledged by other social classes and Kammi respondents themselves emphasize their dependency on their ‘masters’, failing to demarcate the boundaries between their own interests and those of these higher caste families.

A more nuanced analysis shows that this Kammi poverty is the result of deeply entrenched caste based inequities, consequent landlessness and a devaluation of a group of people. In such social and economic circumstances, the most rational strategy during pregnancy is to avoid seeking any form of antenatal care and deliver at home, attended by relatives or traditional birth attendants called the ‘dai’. The existence of maternal health services in the neighbourhood and knowledge of the importance of skilled birth attendance or facility delivery is irrelevant, since they cannot financially or socially access the geographically accessible health facilities. Plus Kammi women expressed a deep mistrust of government services and cited many examples of abusive treatment based on their stigmatized social status. Their inability to accumulate cash reserves and their extreme vulnerability to the benevolence to their ‘wade log’ (the higher social classes) are highlighted most in emergency situations that often result in maternal deaths; deaths that are accepted with a resignation to fate and destiny.
REAL MEDICINE FOUNDATION PAKISTAN
Initiatives
- Disaster Relief
- Hospital & Clinic Projects Support
- Education & School Support
- Refugee Support
- Malnutrition Eradication
- mHealth Programs
- Healthcare Education & Outreach
- Healthcare Capacity Building & Systems
- Economic Stability & Livelihood
- Flood Victims Healthcare Outreach
- Health Research
- HIV/AIDS Prevention & Treatment
- Medical Support
- Mobile Clinics
- Psychological Support
Designed & Developed by Socialoctors
